What you can do to prevent dementia

Dementia affects many people in advanced age. A long-term study in Leipzig, which examined 1,265 seniors aged 75 and older in their home environment, came to the conclusion that five percent of the 75 to 79 year old seniors and even half of the over 90 year old persons suffer from some form of dementia. Even though Alzheimer’s disease is considered the most common form of dementia, most of the elderly suffer from mixed forms, for which not only the changes typical for Alzheimer’s but also vascular-related changes in the brain are responsible.
Dementia can affect anyone. There are many reasons. While dementia diseases were formerly regarded as diseases of the elderly, today the entire life cycle of those people affected is increasingly being considered. It is now known that dementia develops unveiled for decades.
Dementia is currently not curable. As a result, experts are particularly concerned with maintaining cognitive performance and preventing dementia. We now know that there are a number of risk and protective factors that we can influence. Most of the information on these factors comes from studies in which a large number of study participants were observed for a very long time – so-called cohort studies.
The good news: everyone can do something to strengthen his mental fitness. Dementia prevention should start early. What can you do?
Also read the following:
(„Geistig fit ins Alter: Was Sie zur Demenzprävention beitragen können“) unserer Preisträgerin Prof. Dr. med. Steffi G. Riedel-Heller (PDF-Dokument, 3.3 MB)
Lots of exercise, an active social life and intellectual challenges in work and leisure: a healthy lifestyle can reduce the risk of later developing dementia. What can you do to stay mentally fit in old age?
1. Get physically active: Every step is worth it!
People who do sports and exercise regularly are more likely to maintain cognitive performance than those who do not. This is not only said by individual studies, but also by numerous so-called meta-analyzes that summarize the results of many individual studies. Movement protects against loss of cognitive functions and people who move have a lower risk of later developing dementia.
Generally one assumes: the more movement, the better. Ultimately, however, the question has not yet been finally answered as to which physical activities, in what intensity and in what duration or frequency have a special protective effect. There is evidence that physical exertion, e.g. cycling, hiking or gardening, already have an effect once a week.
Even starting small is worthwhile, because there are also indications that people with only minor physical activity have a lower risk of dementia compared to those without any physical activity. Every step is worth it!
Our tip: use a pedometer! Perhaps your smartphone also has such a function. Studies show that just wearing a pedometer motivates you to exercise more.
2. Integrate yourself socially
Humans are social beings. Social activities help to stay mentally fit and reduce the risk of dementia. A meta-analysis of many large cohort studies shows this impressively: low levels of social participation, few social contacts and loneliness increase the risk of later dementia. A larger social network, on the other hand, appears to make a positive contribution to maintaining the cognitive functional level to elderly people. The quality of the relationships is also important.
Older people in particular often have to accept changes and losses. Amongst other things retirement or death of close relatives or friends. Intensive social contacts and the fight against loneliness are very important in this phase of life.
3. Increase your cognitive reserve
A so-called “cognitive reserve” is built up through education, mental demands at work, but also through mentally demanding leisure activities. This can be thought of as a buffer that protects against mental degradation. If degradation processes begin, people with a high cognitive reserve are affected less strong and less quickly. Because they have more reserves, they can maintain their mental performance.
The other side of this coin: Lower education is associated with an increased risk of developing dementia. For each additional year of education, the risk of dementia is reduced by seven percent. A German study showed that an educational path of at least ten years or degrees at technical schools, universities and vocational academies reduce the risk of dementia. But education also protects against dementia at an advanced age: Those who learn lifelong receive their cognitive performance longer.
For many people, the job fills a large part of their lifetime. Workplace challenges can have a positive effect on mental fitness in old age and protect against dementia. This phenomenon has so far been underestimated and has only recently become the focus of research. Jobs that are characterized by complexity, variety and self-determination are advantageous. These findings should also be included in the future design of our working world.
But the risk of dementia can also be counteracted in leisure time. Active participation in mentally demanding leisure activities in the middle of life, but also at an old age, can prevent an increased risk of Alzheimer’s disease and dementia in the elderly. This is proved by several studies. Mentally demanding leisure activities include reading newspapers or books, playing games (e.g. chess or card games, crossword puzzles, going to the theater or performing art).
These effects suggest cognitive training e.g. as a group offer or as a computer-based training for society as a whole. However, the research situation on this is not uniform. Dutch researchers have shown in a literature review that certain areas such as e.g. memory, logical thinking, attention or process speed improve through such training. We assume that the possibilities of computer-based programs, which enable a playful and motivating training of cognitive functions, will be explored more in the future.
Sources:
1. Get physically active: Every step is worth it!
Beydoun MA, Beydoun HA, Gamaldo AA, Teel A, Zonderman AB, Wang Y (2014) Epidemiologic studies of modifiable factors associated with cognition and dementia: systematic review and meta-analysis. BMC Public Health 14:643.
Blondell SJ, Hammersley-Mather R, Veerman JL (2014) Does physical activity prevent cognitive decline and dementia?: A systematic review and meta-analysis of longitudinal studies. BMC Public Health 14:510.
Deckers K, van Boxtel, Martin P J, Schiepers OJG, Vugt M de, Munoz Sanchez JL, Anstey KJ et al (2015) Target risk factors for dementia prevention: a systematic review and Delphi consensus study on the evidence from observational studies. Int J Geriatr Psychiatry 30(3):234–46.
Etgen T, Sander D, Huntgeburth U, Poppert H, Förstl H, Bickel H. Physical activity and incident cognitive impairment in elderly persons: the INVADE study. Arch Intern Med. 2010 Jan 25;170(2):186-93.
Guure CB, Ibrahim NA, Adam MB, Said SM (2017) Impact of Physical Activity on Cognitive Decline, Dementia, and Its Subtypes: Meta-Analysis of Prospective Studies. Biomed Res Int 2017:9016924.
Hamer M, Chida Y. Physical activity and risk of neurodegenerative disease: a systematic review of prospective evidence. Psychol Med. 2009 Jan;39(1):3-11.
Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D et al (2017) Dementia prevention, intervention, and care. The Lancet 390(10113):2673–734.
Llamas-Velasco S, Contador I, Villarejo-Galende A, Lora-Pablos D,Bermejo-Pareja F. Physical Activity as Protective Factor against Dementia: A Prospective Population-Based Study (NEDICES). J Int Neuropsychol Soc. 2015 Nov;21(10):861-7.
Reiner M, Niermann C, Jekauc D, Woll A (2013) Long-term health benefits of physical activity–a systematic review of longitudinal studies. BMC Public Health 13:813.
Sofi F, Valecchi D, Bacci D, Abbate R, Gensini GF, Casini A, Macchi C. Physical activity and risk of cognitive decline: a meta-analysis of prospective studies. J Intern Med. 2011 Jan;269(1):107-17.
Stephen R, Hongisto K, Solomon A, Lonnroos E (2017) Physical Activity and Alzheimer’s Disease: A Systematic Review. J Gerontol A Biol Sci Med Sci 72(6):733–9.
2. Integrate yourself socially
Amieva H, Stoykova R, Matharan F, Helmer C, Antonucci TC, Dartigues JF. What aspects of social network are protective for dementia? Not the quantity but the quality of social interactions is protective up to 15 years later. Psychosom Med.2010 Nov;72(9):905-11.
Crooks VC, Lubben J, Petitti DB, Little D, Chiu V. Social network, cognitive function, and dementia incidence among elderly women. Am J Public Health. 2008 Jul;98(7):1221-7.
Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. 2000 Apr 15;355(9212):1315-9.
Kuiper JS, Zuidersma M, Oude Voshaar RC, Zuidema SU, van den Heuvel, Edwin R, Stolk RP et al (2015) Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev 22:39–57.
Rodriguez FS, Pabst A, Luck T, König HH, Angermeyer MC, Witte AV, Villringer A, Riedel-Heller SG. Social Network Types in Old Age and Incident Dementia. J Geriatr Psychiatry Neurol. 2018 Jul;31(4):163-170.
3. Increase your cognitive reserve
Beydoun MA, Beydoun HA, Gamaldo AA, Teel A, Zonderman AB, Wang Y (2014) Epidemiologic studies of modifiable factors associated with cognition and dementia: systematic review and meta-analysis. BMC Public Health 14:643.
Meng X, D’Arcy C. Education and dementia in the context of the cognitive reserve hypothesis: a systematic review with meta-analyses and qualitative analyses. PLoS One. 2012;7(6):e38268.
Reijnders J, van Heugten C, van Boxtel M. Cognitive interventions in healthy older adults and people with mild cognitive impairment: a systematic review.Ageing Res Rev. 2013 Jan;12(1):263-75.
Stern C, Munn Z. Cognitive leisure activities and their role in preventing dementia: a systematic review. Int J Evid Based Healthc. 2010 Mar;8(1):2-17.
Some physical illnesses such as diabetes, obesity, or depression can pose a risk of cognitive impairment and dementia.
1. Hypertension
High blood pressure is associated with a risk of cognitive disorders and dementia in old age, especially if it occurs in the middle of life. This applies to vascular dementias, but also to Alzheimer’s dementias. High blood pressure should therefore be treated consistently because it can reduce the risk of dementia.
Hinweis: Auf der deutschen Seite steht unter dem Absatz “Bluthochdruck” das Wort “Quellen”. Bitte löschen.
2. Diabetes
The presence of diabetes (diabetes mellitus), especially type 2 diabetes (age-related diabetes), is a risk constellation for the development of dementia. A German study revealed an interesting finding: The diagnosis of type 2 diabetes per se does not increase the risk, rather people have a higher risk of dementia if their blood sugar is insufficiently controlled. This underlines the need for consistent treatment through lifestyle changes and, if necessary, medicinal blood sugar control.
3. Obesity
Obesity in middle age is clearly associated with an increased risk of dementia at an advanced age. Measures taken against increased body weight in middle age can also minimize the risk of dementia. If you want to know exactly whether you are considered normal weight, overweight or obese, you can determine your body mass index (BMI) (Link hinterlegen!) here. Morbid overweight is a chronic condition that can have many causes. Seek medical help – if necessary in special ambulance clinics (Link hinterlegen!).
Hinweis: Auf der deutschen Seite steht unter dem Absatz “Bluthochdruck” das Wort “Quellen”. Bitte löschen.
4. Hearing impairment
First results also indicate a connection between hearing impairment and later dementia development. Because the exact mechanisms have not yet been clarified, we do not know whether the use of hearing aids can really delay the occurence of dementia. Nevertheless, you should have a hearing impairment clarified by a doctor and, if necessary, use aids (e.g. hearing aids).
5. Depression
The connection between depression and dementia has many facets. But it is becoming increasingly clear that depression in earlier adulthood increases the risk of dementia in older age. If the depression only occurs in old age, this is less clear. For example, it is also assumed that depression can also be a so-called prodrome, i.e. precursor to dementia.
6. Beware of drugs with anticholinergic effects
Caution should be exercised with medications with an anticholinergic effect. Medicines with an anticholinergic effect are e.g. used in neurology, psychiatry or internal medicine and taken by 13 percent of older people in Germany. The benefits of these active ingredients are undisputed, they are important and effective drugs. Nevertheless, there are first indications of an increased risk of dementia when used in old age.
For this reason, anticholinergic substances have found their way into a list of medications (PDF document – hinterlegen!) that may be problematic for the elderly. In general, it can be said that older people should be given anticholinergic drugs with extreme caution. Weigh it up with your doctor and look for alternative medications if necessary.
Sources
1. Hypertension
Deckers K, van Boxtel, Martin P J, Schiepers OJG, Vugt M de, Munoz Sanchez JL, Anstey KJ et al (2015) Target risk factors for dementia prevention: a systematic review and Delphi consensus study on the evidence from observational studies. Int J Geriatr Psychiatry 30(3):234–46.
Levi Marpillat N, Macquin-Mavier I, Tropeano A, Bachoud-Levi A, Maison P (2013) Antihypertensive classes, cognitive decline and incidence of dementia: a network meta-analysis. J Hypertens 31(6):1073–82.
Rouch L, Cestac P, Hanon O, Cool C, Helmer C, Bouhanick B et al (2015) Antihypertensive drugs, prevention of cognitive decline and dementia: a systematic review of observational studies, randomized controlled trials and meta-analyses, with discussion of potential mechanisms. CNS Drugs 29(2):113–30.
Sharp SI, Aarsland D, Day S, Sønnesyn H; Alzheimer’s Society Vascular Dementia Systematic Review Group, Ballard C. Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2011.
Jul;26(7):661-9.
2. Depression
Chatterjee S, Peters SAE, Woodward M, Mejia Arango S, Batty GD, Beckett N et al (2016) Type 2 Diabetes as a Risk Factor for Dementia in Women Compared With Men: A Pooled Analysis of 2.3 Million People Comprising More Than 100,000 Cases of Dementia. Diabetes Care 39(2):300–7.
Deckers K, van Boxtel, Martin P J, Schiepers OJG, Vugt M de, Munoz Sanchez JL, Anstey KJ et al (2015) Target risk factors for dementia prevention: a systematic review and Delphi consensus study on the evidence from observational studies. Int J Geriatr Psychiatry 30(3):234–46.
Ramirez A, Wolfsgruber S, Lange C, Kaduszkiewicz H, Weyerer S, Werle J, Pentzek M, Fuchs A, Riedel-Heller SG, Luck T, Mösch E, Bickel H, Wiese B, Prokein J, König HH, Brettschneider C, Breteler MM, Maier W, Jessen F, Scherer M; AgeCoDe
Study Group. Elevated HbA1c is associated with increased risk of incident dementia in primary care patients. J Alzheimers Dis. 2015;44(4):1203-12.
Zhang J, Chen C, Hua S, Liao H, Wang M, Xiong Y et al (2017) An updated meta-analysis of cohort studies: Diabetes and risk of Alzheimer’s disease. Diabetes Res Clin Pract 124:41–7.
3. Obesity
Albanese E, Launer LJ, Egger M, Prince MJ, Giannakopoulos P, Wolters FJ et al (2017) Body mass index in midlife and dementia: Systematic review and meta-regression analysis of 589,649 men and women followed in longitudinal studies. Alzheimers Dement (Amst) 8:165–78.
Pedditizi E, Peters R, Beckett N (2016) The risk of overweight/obesity in mid-life and late life for the development of dementia: a systematic review and meta-analysis of longitudinal studies. Age Ageing 45(1):14–21.
Emmerzaal TL, Kiliaan AJ, Gustafson DR (2015) 2003-2013: a decade of body mass index, Alzheimer’s disease, and dementia. J Alzheimers Dis 43(3):739–55.
4. Hörbeeinträchtigungen
Zheng Y, Fan S, Liao W, Fang W, Xiao S, Liu J. Hearing impairment and risk of Alzheimer’s disease: a meta-analysis of prospective cohort studies. Neurol Sci.2017 Feb;38(2):233-239.
Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, Ballard C, Banerjee S, Burns A, Cohen-Mansfield J, Cooper C, Fox N, Gitlin LN, Howard R, Kales HC, Larson EB, Ritchie K, Rockwood K, Sampson EL, Samus Q, Schneider LS,Selbæk G, Teri L, Mukadam N. Dementia prevention, intervention, and care. Lancet.2017 Dec 16;390(10113):2673-2734.
5. Depression
Bennett S, Thomas AJ. Depression and dementia: cause, consequence or coincidence? Maturitas. 2014 Oct;79(2):184-90.
Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011 May 3;7(6):323-31.
Cherbuin N, Kim S, Anstey KJ. Dementia risk estimates associated with measures of depression: a systematic review and meta-analysis. BMJ Open. 2015 Dec 21;5(12):e008853.
Jorm AF. Is depression a risk factor for dementia or cognitive decline? A review. Gerontology. 2000 Jul-Aug;46(4):219-27.
Heser K, Tebarth F, Wiese B, Eisele M, Bickel H, Köhler M, Mösch E, Weyerer S, Werle J, König HH, Leicht H, Pentzek M, Fuchs A, Riedel-Heller SG, Luppa M, Prokein J, Scherer M, Maier W, Wagner M; Age CoDe Study Group. Age of major depression onset, depressive symptoms, and risk for subsequent dementia: results of the German study on Ageing, Cognition, and Dementia in Primary Care Patients (AgeCoDe). Psychol Med. 2013 Aug;43(8):1597-610.
6. Vorsicht bei Medikamenten mit anticholinerger Wirkung
Gray SL, Anderson ML, Dublin S, Hanlon JT, Hubbard R, Walker R, Yu O, Crane PK, Larson EB. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. 2015 Mar;175(3):401-7.
Gray SL, Hanlon JT. Anticholinergic medication use and dementia: latest evidence and clinical implications. Ther Adv Drug Saf. 2016 Oct;7(5):217-224.
Heser K, Luck T, Röhr S, Wiese B, Kaduszkiewicz H, Oey A et al (2018) Potentially inappropriate medication: Association between the use of antidepressant drugs and the subsequent risk for dementia. J Affect Disord 226:28–35.
Jessen F, Kaduszkiewicz H, Daerr M, Bickel H, Pentzek M, Riedel-Heller S et al (2010) Anticholinergic drug use and risk for dementia: target for dementia prevention. Eur Arch Psychiatry Clin Neurosci 260 Suppl 2:S111-5.
A task for the whole society
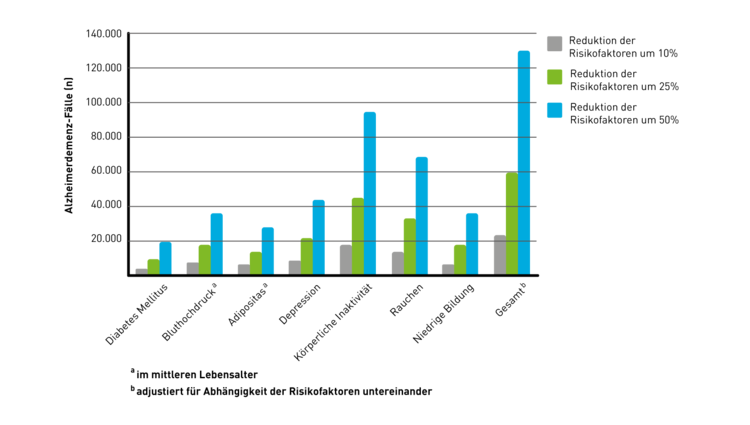
„Predictions are difficult, especially when they concern the future.“ It is not clear who this quote originally came from. The only thing that is clear is that we are very interested in the future. From the point of view of public health, it is interesting, for example, what consequences a reduction in the known and influenceable risk factors for dementia could have. Various projections have already dealt with this question. A prognosis: A 10 to 50 percent reduction in seven risk factors would prevent a noticeable proportion of dementia cases.
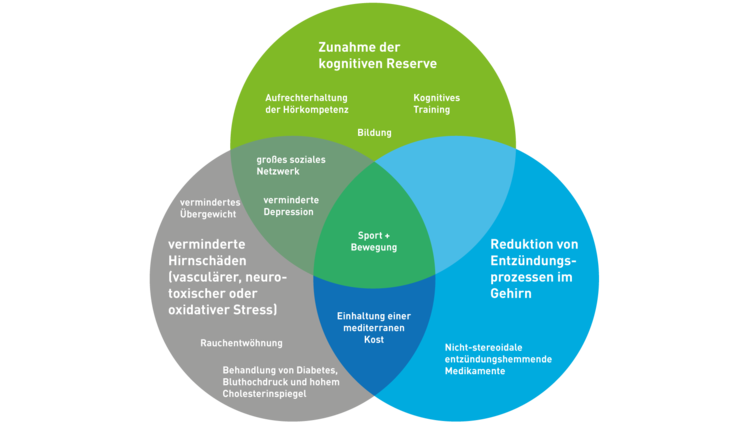
Which mechanisms play a role in prevention?
Of course, you want to know exactly how prevention works: Why does sport and exercise, for example, strengthen our mental fitness? A lot of research is done here. Various mechanisms are discussed for the individual influenceable risk factors, which are summarized in a simplified manner in the following figure.
Prevention in society: do we need a brain health agenda?
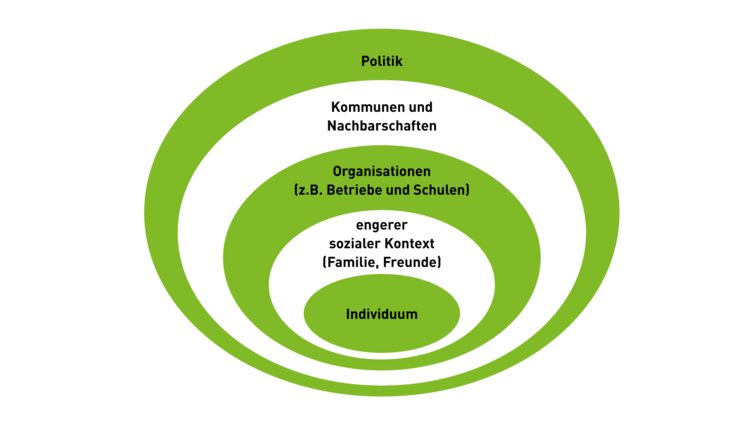
People are social beings and embedded in social contexts, in families, in organizations (e.g. schools, companies), in neighborhoods, communities and entire societies. How important should dementia prevention be in these groups? Let us take the example of sport and physical activity promotion: Yes, the individual can do something – for example, he/she acquires a pedometer and sets a step goal. It is easier if friends motivate or accompany them.
But the environment also plays a role: has the basis been laid in school for a more eventful life? Are there sports clubs and offers for seniors? Are there enough bike paths that make it easier to switch from car to bike? Are there footpaths and parks for Nordern Walking or walking? This example quickly shows that dementia prevention is not only a question of personal lifestyle, but also a task for society as a whole.
Socio-ecological models consider the individual in the area of tension of his direct and distant environment. Socio-ecological prevention models therefore take into account both the behavior of the individual and the effects of their living conditions. These models impressively indicate that successful prevention is always a combination of behavioral and relationship prevention. They give us an idea of how a dementia-preventive environment can be designed. Unfortunately, we are only at the beginning with these considerations.
Sources
Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data. Lancet Neurol. 2014 Aug;13(8):788-94.
Luck T, Riedel-Heller SG. Prävention von Alzheimer-Demenz in Deutschland. Eine Hochrechnung desmöglichen Potenzials der Reduktion ausgewählter Risikofaktoren Nervenarzt. 2016 Nov;87(11):1194-1200
Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S. G., Huntley, J., Ames, D. et al. (2017). Dementia prevention, intervention, and care. The Lancet, 390 (10113), 2673–2734.
Hussenoeder FS, Riedel-Heller SG. Primary prevention of dementia: from modifiable risk factors to a public brain health agenda? Soc Psychiatry Psychiatr Epidemiol. 2018 Dec;53(12):1289-1301.
Pratt M, Perez LG, Goenka S, Brownson RC, Bauman A, Sarmiento OL et al (2015) Can population levels of physical activity be increased? Global evidence and experience. Prog Cardiovasc Dis 57(4):356–67.
McLeroy KR, Bibeau D, Steckler A, Glanz K et al (1988) An Ecological Perspective on Health Promotion Programs. Health education quarterly 15 (4):351–377.
